Each year the Centers for Medicare and Medicaid Services review proposed changes to the Medicare program. The CMS 2024 final rule will most impact agents and third-party marketing organizations.
The 2024 final rule requires a minimum 48-hour window between a Scope of Appointment form being completed and an appointment taking place. It also limits how long agents or TPMOs can contact a beneficiary after requesting they request information.
What’s included in the 2024 CMS Final Rule?
The CMS final rules affect Medicare beneficiaries, providers, insurance companies, agents (brokers), and Third-party marketing organizations (TPMOs). We’ll give an overview of the changes and who it affects.
Some of the biggest changes include a mandatory minimum 48-hour waiting period between the signing of a Scope of Appointment (SOA) form, limiting permission to contact to a 6-month maximum, annual opt-out requirement, prohibition of the marketing of savings not realized, and the requirement of identifying of carriers represented in marketing materials.
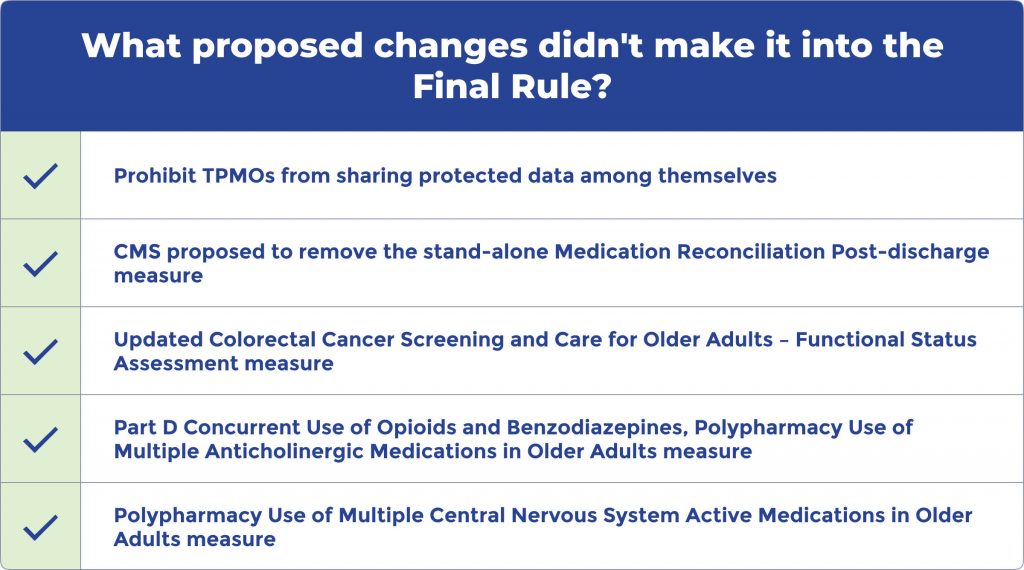
What proposed changes didn’t make it into the final rule?
Some proposed changes didn’t make it into the 2024 Final Rule. Among the most notable proposed changes were the following:
- Prohibit TPMOs from sharing protected data among themselves
- CMS proposed to remove the stand-alone Medication Reconciliation Post-discharge measure
- The stand-alone Medication Reconciliation Post-discharge measure is a quality measure that assesses the performance of healthcare providers in reconciling medication information for patients after they are discharged from a hospital or other care facility.
- Updated Colorectal Cancer Screening and Care for Older Adults – Functional Status Assessment measure
- The Functional Status Assessment measure is used in healthcare to assess a patient’s ability to perform activities of daily living and determine their level of independence.
- Part D Concurrent Use of Opioids and Benzodiazepines, Polypharmacy Use of Multiple Anticholinergic Medications in Older Adults measure
- This quality measure is used in Medicare Part D plans to assess the safety and appropriateness of medication use in older adults.
- Polypharmacy Use of Multiple Central Nervous System Active Medications in Older Adults measure
- This quality measure assesses the percentage of patients 65 years and older who have been prescribed two or more CNS-active medications for at least 90 days during the measurement year.
Effects of the 2024 CMS Final Rule
Changes in the 2024 CMS Final Rule will impact all parties involved with Medicare, from beneficiaries to doctors, insurance companies, brokers, and marketing companies. Many of these changes are positive for Americans enrolled in Medicare. However, some items included in the final rule will impact how the enrollment marketing changes will significantly impact insurance companies, brokers, and marketing organizations.
2024 Changes to marketing rules
One of the biggest impacts comes in the form of marketing changes. Below we’ll discuss these changes and how they will impact insurance companies, providers, and TPMOs.
Ban the promotion of unrealized savings
Many use the potential benefits of Medicare Advantage plans as a tool to get beneficiaries to call in, fill out lead forms, or other methods to collect lead data. Many advertisements advertise these savings benefits, such as the $900 food card, but these benefits are only available in some areas. The new rules prohibit marketing unavailable benefits or savings.
Permission to contact and opt-out changes
Before the rule change, once permission to contact had been given in any form, that permission was ongoing, and beneficiaries were getting calls about requests made several months and even years prior. All ways of collecting permission to contact will now have a limit of 6 months. In addition, insurance companies must provide Medicare beneficiaries with a one-time opt-out chance annually. By doing this, the insurance company will remind its beneficiaries that they have the right to choose not to receive any communications regarding plan business.
48-hour cooling-off period for SOA and meetings
Under the new 2024 rules, there is a required 48-hour cooling-off period between completing the SOA form and the actual meeting between the beneficiary and broker. This allows Medicare members to speak with caregivers or whoever helps them make their Medicare decisions.
Identification of plan sponsors in marketing materials
This new rule will require these sponsoring organizations to be identified in 12-point font in all print advertisements. This identification must be displayed in areas other than the fine print and disclaimer section. And must mention all Medicare Advantage and Part D plan sponsors and the TPMO.
For online, TV, or social media advertisements, the names must be displayed during the entire advertisement or read within the advertisement at the same pace as the advertised benefits or phone numbers. Centers for Medicare & Medicaid Services implemented these changes to give the beneficiary “Necessary and appropriate information to decide” if they want to contact the plan or TPMO based on the organizations represented.
Submitting Advertising Materials
Before using any creatives for marketing and advertisements, they must be approved by CMS. This new rule focusing on TPMOs must receive prior approval from the MA and PDP Plan sponsors before submitting materials through the Health Plan Management System (HPMS).
Call recordings
Centers for Medicare & Medicaid Services has rolled back the change from last year, requiring recordings of all calls to only calls related to marketing, sales, and enrollment. There was also clarification that the recoding requirements include web technology such as Zoom and GoogleMeets.
Additional finalizations to improve the quality of care
Prior Authorization for coordinated care plans.
When it comes to coordinated care plans, prior authorization is a process that allows the insurance company to confirm that you have a certain health condition or that a specific treatment or service is medically necessary for you.
It’s important to know that insurance companies can only use prior authorization to ensure you receive the care you need. They can’t use it for any other reason.
For example, if you need a medication or medical procedure, your insurance company may require prior authorization to ensure it’s appropriate and necessary for your health.
If you have any questions or concerns about prior authorization, talk to your doctor or contact your insurance company for more information
Requirement of MA plans to comply with national and local coverage determinations
If you have a Medicare Advantage (MA) plan, it’s important to know that the Centers for Medicare & Medicaid Services require these plans to follow certain rules about what they cover.
For example, these rules include ‘national coverage determinations’ (NCDs) and ‘local coverage determinations’ (LCDs). These criteria help determine if Traditional Medicare covers a medical service or item.
Your MA plan must also comply with general coverage and benefit conditions that are part of Traditional Medicare laws. This means that the same rules apply to Traditional Medicare to MA plans.
However, it’s important to note that CMS is not changing the existing ‘step therapy’ policies for Part B drugs. This means that your MA plan may still require you to try certain drugs before they cover a different one.
Allow plans to develop internal coverage criteria for medical necessity determinations when no applicable Medicare statute exists
Sometimes there may not be clear rules about whether your Medicare Advantage (MA) plan covers a certain medical service or item. In those cases, CMS will allow your plan to create its own ‘coverage criteria’ to help make a decision.
However, your plan must make these criteria available to you and the public so you know what they are. They must also use current evidence from well-known medical guidelines or literature to make these criteria.
If additional criteria aren’t included in the rules, the MA organization must help you more than harm. For example, they need to show that delays or reduced access to medical services or items will not harm you more than the benefit you’ll receive.
Approval of prior authorization processes
When a company approves a prior authorization, CMS now requires that it remain valid for as long as it is medically necessary. This ensures continuity of care, considering the patient’s medical history, the applicable coverage criteria, and the treating provider’s recommendations.
Additionally, plans must provide a minimum of 90 days to transition to a new MA plan, switch from Traditional Medicare to an MA plan, or join Medicare while receiving active treatment. This is to prevent any interruptions in the patient’s care.
Requirement all MA plans to establish a Utilization Management Committee
The new CMS rules for 2024 will mandate that all MA plans must set up a Utilization Management Committee. This committee will review policies once a year to ensure they align with Traditional Medicare’s NCDs, LCDs, and guidelines.
The medical director will head the committee. It will mainly consist of practicing physicians, with at least one independent physician free from conflict with the MA organization or plan. Additionally, at least one physician must be an expert in providing care to the elderly or disabled, The committee should include members from diverse clinical specialties.
FAQ
What’s the final rule for CMS 2024
Each year CMS reviews the state of Medicare and reviews proposals for changes to the program. The final rule is the approved changes, which will be implemented for the following year.
Does Medicare have a lifetime maximum?
No, Medicare doesn’t have a lifetime maximum for services covered by Medicare at Medicare-approved providers. However, Medicare also has no cap on how much you can spend. This is why many Medicare beneficiaries enroll in a Medicare Supplement or Medicare Advantage plan.
What income is used to determine Medicare premiums for 2024?
We rely on the latest tax return the IRS provides to determine your eligibility for premium subsidies. If your income exceeds a certain threshold, you may pay higher premiums, calculated based on a sliding scale that considers your modified adjusted gross income (MAGI). This includes all of your taxable income and any tax-exempt interest income.
Can Medicare Advantage companies cold call me to try and sell me a plan?
No. For a Medicare Advantage company to initiate a phone call, they must have permission to fill out the contact form. The new 2024 CMS Final Rule aims to combat illegal practices from bad actors.
When looking for the right Medicare plan for your needs, it’s crucial to have accurate information on benefits, networks, and costs. To review plans in your area, simply fill out our online rate form or call us. We look forward to making your Medicare experience quick and painless.
Methodology
Medigap.com extracted and analyzed data from the following to provide data in this article.
- “2024 Medicare Advantage and Part D Final Rule” (CMS)
- “CMS’ 2024 Final Notice and Rule: What You Need to Know” (Healthmine)
- “Key Takeaways from the 2024 MA Final Rule” (ForeSee Medical)
Related Links
- 2023 Medicare Parts A & B Premiums and Deductibles IRMAA
- What to Expect with the Medicare Part B Decreases for 2023
- How Price Transparency Would Impact Medicare Beneficiaries
- The State of Medicare & Social Security
- Medicare Advantage Plans Deny Needed Care
- Medicare Announces First 10 Drugs for Price Negotiations