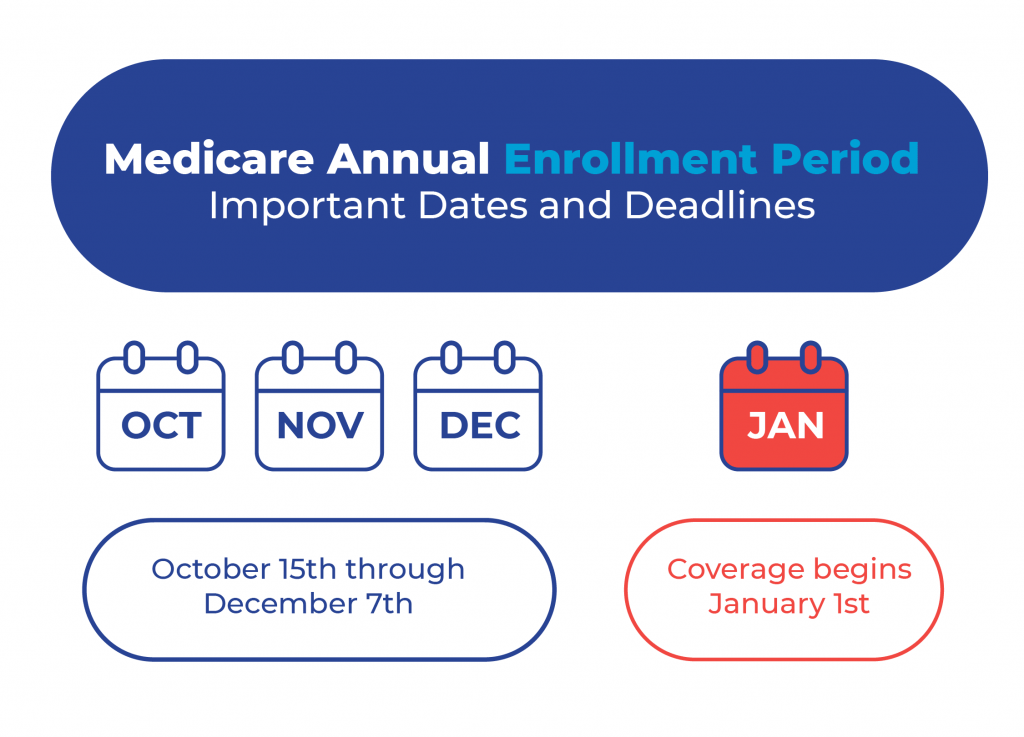
We all know that the Medicare Annual Enrollment Period occurs in the fall. Even individuals not on Medicare know based on the influx of advertisements everywhere you turn. However, sometimes life does get in the way, and people forget or miss the window. Next, we’ll discuss what Medicare beneficiaries can do if they miss AEP.
What If I Miss the Annual Enrollment Period?
A few things could happen, and it revolves around the current coverage. Depending on what coverage you currently have depends on what will happen. Most individuals with Medicare benefits have a Medicare Advantage Plan or Original Medicare with Part D prescription drug plan with a Medicare Supplement insurance policy.
Medigap plans aren’t affected by the Annual Election Period. You can change or start a Medicare Supplement plan anytime if your health permits. However, you can’t simultaneously be on a Medicare Advantage plan and Medigap policy.
Suppose you’re enrolled in an MAPD and want a Medicare Supplement. In that case, you’ll have to be able to drop your Medicare Advantage plan before your Medicare Supplement can start.
Missing AEP With a Medicare Advantage Plan
Beneficiaries enrolled in Medicare Advantage plans can make changes during the AEP. If you miss the Annual Enrollment Period, your current plan will roll over to the new plan.
The exception is if your current Medicare Advantage plan leaves the services area or gets discontinued. If this occurs, you’ll have a Special Enrollment Period lasting two months after the Part C program ends.
With enrollment in a Medicare Advantage plan, as long as you’re actively enrolled, you can change the Medicare Advantage Open Enrollment Period. The MAOEP runs from January 1st until March 31 annually.
During this enrollment period, you can change your Medicare Advantage plan. If you miss the AEP and MAOEP, you will be locked in your current plan unless you have a qualifying Special Enrollment Period.
Suppose you’re on Original Medicare only and miss the Annual Enrollment Period. In that case, you won’t be able to add a Medicare Advantage plan or a Medicare Part D plan unless you have a Special Enrollment period.
Medicare Advantage Open Enrollment Period
In the MAOEP, you can do the following:
- Drop your current Medicare Advantage plan to return to your Original Medicare
- Enroll in a different Medicare Advantage plan
- Drop your current Medicare Advantage plan, return to Original Medicare, and enroll in a Medicare Part D prescription drug plan
Any plan changes occurring in the MAOEP will take effect on the 1st of the following month. If you enroll in a Medicare Supplement, you can use this OEP to drop the Medicare Advantage plan.
Missing AEP with a Part D Prescription Drug Plan
Like a Medicare Advantage plan, if you miss the AEP, your current plan will roll over to the new year unless the program ends. If you miss the enrollment period and want to change, you’re out of luck unless you have a Special Enrollment Period.
Special Enrollment Period
Certain life events and special circumstances trigger a SEP. Some examples of Special Enrollment Periods include:
- Moving out of your plans coverage area
- Qualifying or losing Medicaid or Extra Help.
- Active Enrollment in Medicaid or low-income programs that pay portions of your Medicare costs.
- Losing or leaving a creditable group or employer coverage
- Loss of your current plan at no fault of your own such as the plan losing or ending its contract with Medicare
- Moving into, out of, or still living in a skilled nursing facility or another institution such as a long-term care hospital.
- Getting out of jail
- Moving back to the United States after living outside the country
These are just a few examples of special circumstances that will cause a SEP. Another Medicare Special Enrollment Period is enrolling in a 5-Star Medicare Advantage plan. Plans that have received this rating can take enrollments between December 8th and November 30th. You can only make this election once in a given year.
Medigap Enrollment if Outside of the Annual Enrollment Period
As mentioned above, Medicare Supplement health insurance isn’t affected by the AEP unless you need to drop your current Medicare Advantage plan. Although you can always change your Medicare Supplement if you can medically qualify, a few times allow enrollment without underwriting.
Medicare Supplements have an Open Enrollment Period when a Medicare beneficiary’s Part B starts or as they approach their 65th birthday. This period lasts for months from the start of Medicare Part B or the 1st of their birth month.
Medicare Supplement insurance plans also have guarantee issue rights that work like a Special Enrollment Period. Seven GI rights allow you to enroll in a Medigap plan without underwriting.
Many Medicare Advantage plan enrollees review Medicare Supplements in AEP since they can drop their MA plan during this time. Suppose a beneficiary is considering a Medigap plan. In that case, enrolling early in the AEP is wise to allow plenty of time for an underwriting decision before dropping their Medicare coverage.
FAQs
What happens If I am denied a Medigap enrollment in AEP?
It’s recommended that if you plan to enroll in a Medigap and drop your Medicare Advantage plan that it’s completed early in an AEP. If you’re denied, you have time to find another Medicare Advantage plan. You should never drop your current plan before your new plan has been approved.
Can I enroll in Medicare Part B during the Medicare Annual Enrollment Period?
The AEP is only for beneficiaries enrolled in Medicare already. Suppose you missed your Initial Enrollment Period (IEP) and don’t qualify for a Special Enrollment Period. In that case, you’ll need to wait until the General Enrollment Period to enroll in Medicare Part B.
Getting Help Navigating the Medicare Annual Enrollment Period
A licensed insurance agent can help you navigate through the craziness of the AEP. They can assist with finding plans that fit your individual needs and guide you through the processes and timeframes involved.
This ensures you complete any changes and don’t miss your opportunity. Give us a call or fill out our online form. Our specialists can help with any Medicare questions or guidance you need.